Multi-Biomarker Detection Biosensors: Quick Diagnosis at Your Fingertips
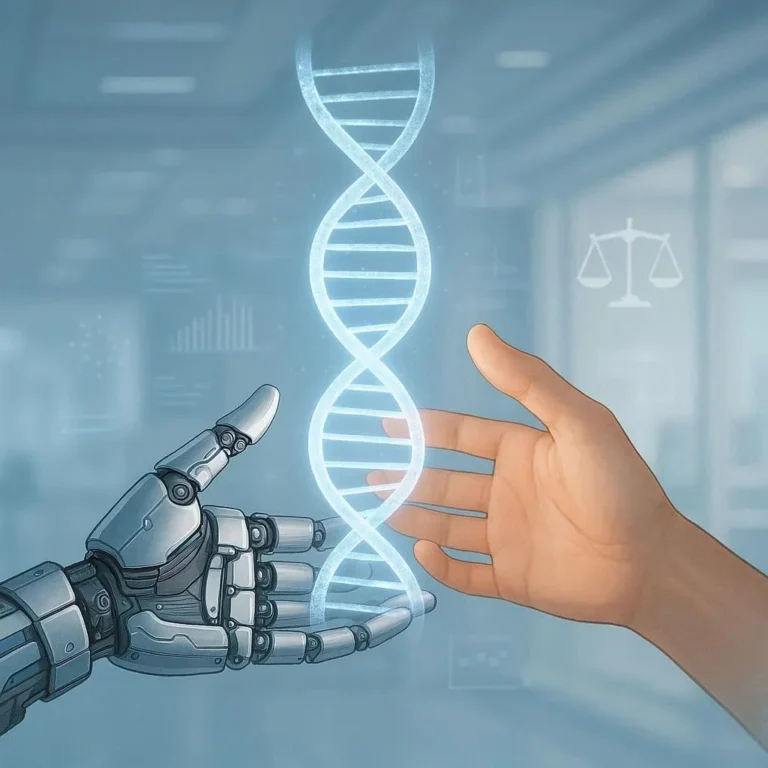
In today’s fast‑moving world, the ability to identify a disease the moment it appears—without waiting in line at a lab—has become a game‑changer for both patients and clinicians. Multi‑biomarker detection biosensors do exactly that by measuring multiple biomarkers in a single, painless test. Rather than testing for one disease marker at a time, these smart devices pull together panels of proteins, metabolites, or nucleic acids that provide a holistic view of your health.
Key Advantages
- Speed: Results in minutes, not days.
- Precision: Multiple biomarkers reduce false positives/negatives.
- Convenience: Finger‑prick or saliva samples eliminate invasive procedures.
- Data‑Driven Insights: Integrated apps and cloud analytics enable continuous monitoring.
- Scalability: Ideal for clinics, community health centers, and even home‑use.
Popular Surrogate Biomarker Panels
| Condition | Typical Biomarkers | Example Biosensor Application |
| Diabetes | HbA1c, glucose, ketones | Rapid glucose‑ketone monitor |
| Cardiovascular | Troponin, CRP, NT‑proBNP | Point‑of‑care cardiac panel |
| Infectious Diseases | CRP, procalcitonin, viral RNA | Early sepsis or COVID‑19 test |
Applications range from detecting heart attack markers in an ambulance to measuring blood sugar during a pandemic’s rapid response.
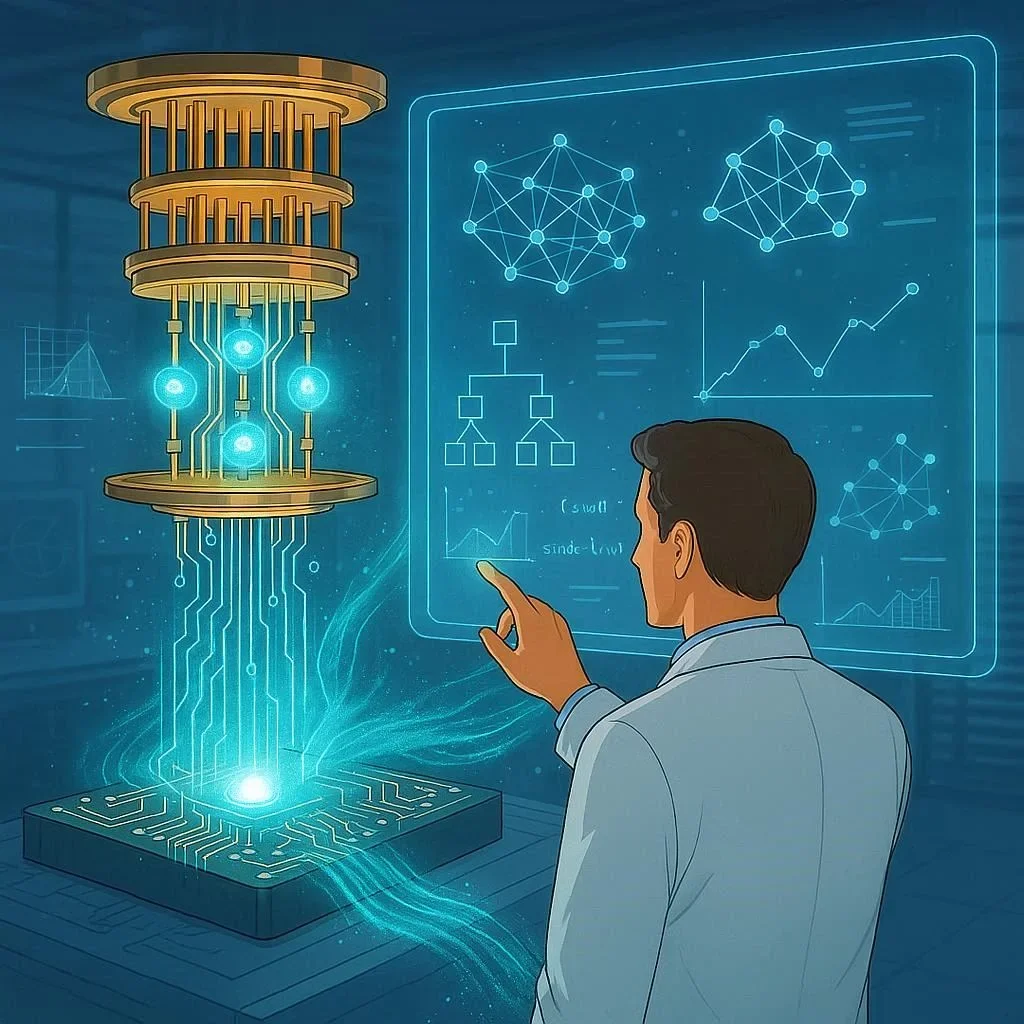
How Multi‑Biomarker Biosensors Work
At the core of these devices lies a sophisticated integration of nanomaterials, bio‑receptors, and electronics. Here’s a simplified breakdown:
- Sample Acquisition – A tiny device collects a blood drop or a saliva sample.
- Bio‑Receptor Layer – Antibodies or aptamers on graphene or gold nanostructures bind specific biomarkers.
- Transduction – Binding events alter electrical, optical, or mass properties that a micro‑electronic circuit detects.
- Signal Amplification – Enzymes or nanoparticles amplify the detection signal, enhancing sensitivity.
- Data Processing – Real‑time algorithms determine biomarker levels and compare them against diagnostic thresholds.
- Communication – Results travel to a smartphone or a cloud server via Bluetooth or Wi‑Fi.
The combination of surface‑enhanced Raman scattering (SERS), electrochemical impedance spectroscopy, and microfluidic pre‑concentration enables some devices to detect concentrations as low as parts per trillion.
Biosensor basics provide the scientific foundation for these next‑generation tools.
From Lab to Clinic: The Validation Journey
Until now, many studies have only shown the analytical performance in vitro. The next step is rigorous clinical validation to prove these biosensors deliver reliable results in real‑world scenarios.
Key Validation Metrics
- Analytical Sensitivity – Limit of detection (LOD) for each biomarker.
- Analytical Specificity – Ability to distinguish target analyte from similar molecules.
- Clinical Sensitivity & Specificity – Accuracy when applied to patient samples.
- Reproducibility – Consistency across batches and over time.
- Regulatory Acceptance – FDA, CE marking, or WHO pre‑qualifications.
Researchers are now partnering with entities like the FDA’s Breakthrough Devices program, enabling faster approval for life‑saving point‑of‑care products.
FDA device approval resources clarify the pathway.
Integrating Biosensors with Smart Technology
Modern resilience to chronic conditions relies heavily on continuous data. High‑throughput biosensors are pairing with wearable sensors, cloud analytics, and AI to offer a seamless health ecosystem.
1. Wearable‑Biosensor Hybrids
Imagine a smartwatch that not only tracks heart rhythm but also delivers a finger‑prick blood test for glucose and CRP on demand. Manufacturers like Abbott and Gravito are exploring such hybrid devices.
2. Cloud‑Enabled Telemedicine
Data from biosensors feeds into secure cloud platforms where clinicians can monitor trends, receive alerts, and adjust treatment plans remotely. This model is essential for pandemic responses and rural healthcare.
3. AI‑Driven Interpretations
Algorithms sift through millions of biomarker readings to spot patterns that a human eye might miss—such as predicting sepsis onset before vital signs change dramatically.
WHO health systems insights emphasize AI’s role in bolstering diagnostic reach.
Real‑World Use Cases: Transforming Patient Experience
| Setting | Biosensor Application | Outcome |
| Emergency Rooms | Rapid troponin & CRP panel | Cuts triage time by 30% |
| Home Monitoring | Diabetes & ketone panel | Enables patients to adjust insulin in real time |
| Outbreak Response | COVID‑19 viral RNA & CRP biosensor | Faster contact tracing for outbreaks |
| Athletes | Hemoglobin & electrolytes panel | Fine‑tunes performance and recovery |
These scenarios show that multi‑biomarker biosensors are not merely technology toys; they’re impactful healthcare tools.
Challenges & Future Directions
1. User Adoption
While these devices are technically elegant, widespread adoption depends on simple user interfaces, affordability, and robust data privacy controls.
2. Complex Panel Design
Creating panels that remain clinically relevant as new biomarkers emerge requires agile development pipelines.
3. Regulatory Complexity
Each biomarker increases the regulatory burden. Harmonizing global standards can accelerate market entry.
4. Economic Sustainability
Hot‑spots for future research include developing reusable sensor platforms to reduce per‑test costs.
Emerging Trends
- Paper‑Based Lab‑On‑Chip devices that are low‑cost and deployable in resource‑poor settings.
- Micro‑RNA Panels for early cancer detection.
- Blockchain Auditing for immutable health data logs.
Making the Leap: How You Can Benefit
If you’re a clinician, a healthcare administrator, or simply a health‑conscious individual, here’s what to do:
- Stay Informed: Subscribe to industry newsletters from Biosensing.org.
- Evaluate Panels: Look for FDA‑cleared or CE‑marked devices that match your patient population.
- Pilot Programs: Test integration with existing EMR systems in a controlled setting.
- Patient Education: Develop clear, jargon‑free guides that illustrate how to use the device and interpret the results.
The Bottom Line
Multi‑biomarker detection biosensors represent the convergence of nanomedicine, data science, and wearable tech. Their ability to deliver rapid, precise, and convenient diagnostic information at the touch of a finger is redefining how we view preventive, point‑of‑care, and chronic disease management.
If you’re ready to leap into the next era of personal health diagnostics, explore the latest biosensors, understand the science behind them, and integrate them into your care model. Your patients—and your own peace of mind—will thank you.