Exploring the Role of Gut Microbiota in Human Health
The Hidden Influence of Our Gut Microbiota
Welcome to the fascinating world where trillions of microbes meet human biology—a dynamic ecosystem that quietly steers every facet of our health. In this post we delve deep into the gut microbiota in human health, uncovering the science, practical implications, and everyday actions that can harmonize this invisible community.
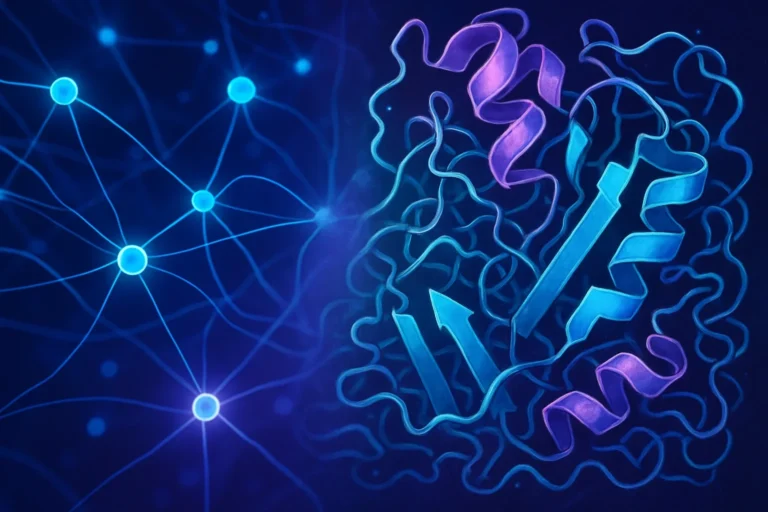
What Is Gut Microbiota? The Living Library Inside Us
The gut microbiota refers to the collective genomes and organisms residing in our gastrointestinal tract. Key facts:
- Bacterial species: Over 1000 distinct species, primarily from the Firmicutes and Bacteroidetes phyla.
- Genetic breadth: Contains ~100 trillion genes—more than human genes combined.
- Functional roles: Digestion, vitamin synthesis, immune modulation, and neurotransmitter production.
For a primer on the microbiome, the Wikipedia article on the microbiome offers a comprehensive overview. The sheer scale of this ecosystem underscores its significance in maintaining physiological equilibrium.
How the Gut Microbiota Interacts With Our Bodies
- Metabolic Powerhouse – Fermentation of dietary fibers produces short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. These molecules fuel colonocytes, regulate glucose metabolism, and influence adiposity.
- Immune Training – Microbial antigens educate immune cells, guiding tolerance to foreign proteins while defending against pathogens.
- Neurological Whisperers – The “gut‑brain axis” showcases bidirectional communication via neurotransmitters, vagus nerve signaling, and the endocrine system.
- Barrier Protectors – Tight-junction proteins form a defensive wall; a balanced microbiota helps maintain barrier integrity, preventing leaky gut syndrome.
The pivotal role of SCFAs in health is highlighted in a landmark 2022 review from the National Institutes of Health, illustrating how deficits correlate with inflammatory bowel disease and metabolic disorders.
Dysbiosis: When Balance Breaks Down
Dysbiosis denotes a disrupted microbial community—a shift that can precipitate disease. Common culprits include:
- Overuse of antibiotics → Rapid loss of beneficial taxa.
- Western diets high in fats and sugars → Reduced diversity.
- Chronic stress and sleep deprivation → Hormonal changes affecting microbial proliferation.
Clinical implications are vast:
- Autoimmune diseases such as Crohn’s disease, rheumatoid arthritis, and multiple sclerosis show strong correlations with altered microbial signatures.
- Metabolic syndrome and obesity often align with increased Firmicutes to Bacteroidetes ratios.
- Mental health disorders (depression, anxiety) are increasingly linked to gut microbial imbalances via the gut‑brain axis.
The American Gut Project, hosted by the American Gut Initiative, underscores how lifestyle factors shape microbial composition and, consequently, disease risk.
Harnessing the Power of Probiotics and Prebiotics
Probiotics: Introducing Beneficial Strains
Probiotics are living microbes that, when ingested in adequate amounts, confer health benefits. Popular strains:
- Lactobacillus rhamnosus GG
- Bifidobacterium longum
- Saccharomyces boulardii (yeast)
Evidence from randomized controlled trials indicates probiotics can:
- Reduce duration of antibiotic-associated diarrhea.
- Mitigate symptoms of irritable bowel syndrome.
- Improve mood metrics in mild depression.
For dosage guidance, consult the World Health Organization’s probiotic guidelines.
Prebiotics: Feeding the Good Guys
Prebiotics are non-digestible fibers that selectively stimulate beneficial microbes. Key sources include:
- Inulin (found in chicory root, garlic, onions)
- Galacto‑oligosaccharides (GOS) in dairy
- Resistant starches in cooled potatoes and legumes
Research reveals prebiotic consumption boosts SCFA production and enhances gut barrier function. A 2023 meta‑analysis (source: Frontiers in Nutrition) reported significant reductions in inflammatory markers among participants consuming prebiotic‑rich diets.
The Gut Microbiome and Immune System Synergy
The immune system spends roughly 70% of its activity within the gut. Microbial signals modulate T helper cells (Th17, Treg), influence cytokine profiles, and regulate innate immune receptors like NLRP3 inflammasome. Disruptions can lead to chronic inflammation and autoimmunity.
Key Mechanisms
- Treg induction: Certain butyrate producers promote regulatory T cells, suppressing inflammation.
- Dendritic cell modulation: Microbial metabolites shape antigen‑presenting cell maturation.
- Pattern‑recognition receptors (PRRs): Bacterial ligands engage Toll‑like receptors, balancing pro‑inflammatory and anti‑inflammatory pathways.
The comprehensive review by Harvard T.H. Chan School of Public Health (link: Harvard Health Blog) offers insight into how diet‑derived microbiota influence systemic immunity.
Gut Microbiota and Metabolic Health
Obesity and Weight Management
Microbiota composition correlates with adiposity. SCFAs act as signaling molecules for leptin and ghrelin, influencing appetite. A balanced microbiome improves insulin sensitivity, thereby reducing type‑2 diabetes risk.
Lipid Metabolism
Certain Lactobacillus species can deconjugate bile acids, affecting cholesterol absorption. Probiotic intake is linked to modest cholesterol reductions in meta‑analyses.
Energy Harvest
An overrepresentation of Firmicutes can enhance caloric extraction from otherwise indigestible polysaccharides, contributing to weight gain. Conversely, a higher Bacteroidetes ratio is associated with lean phenotypes.
The Microbiome‑Brain Axis: Mental Well‑Being
Emerging evidence connects gut health to mood disorders.
- Serotonin production: ~90% of serotonin originates in the gut, guided by microbiota.
- Neurotransmitter synthesis: Certain microbes produce GABA, dopamine precursors, and tryptophan metabolites.
- Inflammation‑mediated pathways: Chronic systemic inflammation from dysbiosis perpetuates depressive symptomatology.
A 2021 clinical trial at the University of California showed that probiotic supplementation reduced anxiety scores in participants over eight weeks (source: NIH PubMed).
Practical Steps to Cultivate a Healthy Microbiome
| Action | Why It Works | Suggested Foods/Practice |
|—|—|—|
| Increase fiber intake | Provides substrate for SCFA production | Berries, oats, legumes, leafy greens |
| Consume fermented foods | Directly introduces live cultures | Sauerkraut, kimchi, kefir, kombucha |
| Avoid unnecessary antibiotics | Preserves microbial diversity | Discuss alternatives with your clinician |
| Manage stress | Lowers cortisol, which adversely influences gut microbes | Meditation, yoga, regular sleep schedule |
| Regular physical activity | Enhances microbial richness | 30 minutes brisk walk daily |
The European Food Safety Authority (EFSA) recommends a minimum of 25 g of fiber per day for adults to support gut health.
Future Horizons: Precision Microbiome Therapies
Technological advancements are ushering in personalized gut health strategies:
- Microbial sequencing to profile individual microbiomes.
- Targeted probiotic consortia tailored to specific health states.
- Fecal microbiota transplantation (FMT), increasingly validated for recurrent Clostridioides difficile infections.
- Prebiotic‑enriched diets guided by metabolomic markers.
Clinical trials, such as those conducted by the Mayo Clinic, are exploring microbiome modulation in depression and cancer immunotherapy, signifying a new frontier in holistic treatment modalities.
Conclusion: Unlocking Health Through Microbial Harmony
The gut microbiota stands as a pivotal determinant of human health—from metabolic regulation and immune defense to mental well‑being. By embracing diet‑rich fibers, fermented foods, reduced antibiotic use, and stress management, we can nurture this microscopic ally.
Take action today: Start incorporating a diverse array of prebiotic foods into your meals, explore probiotic supplements vetted by healthcare professionals, and monitor your gut health with simple at‑home tests. Your microbiome—and your overall wellbeing—will thank you.
Engage with us: share your personal gut‑health journeys in the comments below or try our free microbiome assessment tool linked at the end of this article. Together, let’s champion a healthier future—one gut microbe at a time.
**(Learn more at the American Society for Microbiology and the *Nature Medicine for the latest research insights.)*