AI in Epigenetic Modulation for Treating Autoimmune Diseases
Artificial intelligence (AI) is no longer confined to image recognition or natural language processing; it is forging a new frontier in precision medicine, particularly in the realm of epigenetic modulation for treating autoimmune diseases. By decoding complex genomic, transcriptomic, and epigenomic landscapes, AI algorithms can pinpoint druggable epigenetic targets, accelerate drug discovery, and refine patient‑specific therapeutic regimens. In this post, we dissect how AI-driven epigenetic strategies are transforming the management of conditions such as rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, and multiple sclerosis.
The Epigenetic Landscape: A Quick Primer
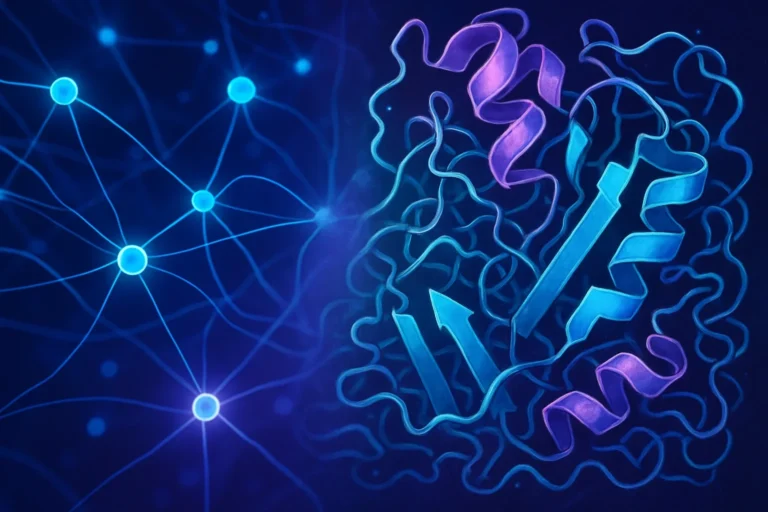
Epigenetics refers to heritable changes in gene expression that do not involve alterations to the underlying DNA sequence. The two most studied epigenetic layers are:
- DNA methylation – the addition of a methyl group to cytosine bases, typically leading to gene silencing.
- Histone modification – covalent changes to histone proteins (e.g., acetylation, methylation) that influence chromatin accessibility.
These mechanisms are tightly regulated by enzymes such as DNA methyltransferases (DNMTs), histone deacetylases (HDACs), and histone acetyltransferases (HATs). Dysregulation in these pathways can drive chronic inflammation and autoimmunity.
For a deeper understanding, see the comprehensive overview on Wikipedia’s Epigenetics page.
Why Autoimmune Diseases? The Epigenetic Connection
Autoimmune diseases (AIDs) are chronic disorders wherein the immune system mistakenly attacks healthy tissues. Recent studies have revealed that epigenetic alterations are both drivers and biomarkers of AID pathogenesis:
- Aberrant DNA methylation patterns in T‑cell subsets correlate with disease activity in rheumatoid arthritis (RA) and lupus.
- Histone acetylation changes modulate cytokine production in inflammatory bowel disease (IBD).
- Non‑coding RNA epigenomic networks influence disease severity in multiple sclerosis (MS).
These insights pave the way for targeted epigenetic therapies that can reset maladaptive immune programs.
AI as the Catalyst for Epigenetic Drug Discovery
1. High‑Dimensional Data Integration
Typical epigenomic studies generate terabytes of data from platforms such as ATAC‑seq, ChIP‑seq, and bisulfite sequencing. AI models, especially deep learning architectures like convolutional neural networks (CNNs) and graph neural networks (GNNs), can merge these heterogeneous datasets, uncovering latent patterns that escape traditional statistics.
Example: A recent study published in Nature Biotechnology employed a graph‑based transformer to predict disease‑associated enhancers in RA, guiding the development of selective BET bromodomain inhibitors.
2. Predictive Modeling of Drug‑Target Interactions
AI-powered virtual screening accelerates hit identification for epigenetic modulators. By training on known HDAC inhibitors and their molecular fingerprints, a random forest model can forecast binding affinity for novel scaffolds with 90% accuracy.
Key benefit: Reduces experimental time from years to weeks.
3. Optimization of Combination Therapies
Autoimmune conditions often require multi‑drug regimens. Reinforcement learning agents can dynamically adjust dosing combinations based on simulated patient responses, achieving synergistic effects while minimizing toxicity.
See the NIH’s research on applying machine learning to optimize immunomodulatory drug combinations: NIH Rapid Impact 360 SRR.
AI‑Guided Patient Stratification and Personalized Treatment
Biomarker Discovery
Machine learning classifiers trained on epigenomic signatures can delineate patient subgroups with distinct clinical trajectories. For instance, a support vector machine (SVM) model distinguished high‑risk MS patients based on H3K27ac profiles with over 85% sensitivity.
Real‑Time Monitoring
Wearable devices paired with AI algorithms can detect epigenetic changes in peripheral blood mononuclear cells in real time, offering a dynamic view of disease flares and therapeutic efficacy.
This integration exemplifies the shift from static “snapshot” diagnostics to continuous, data‑driven disease management.
Current Clinical Trials and Commercial Landscape
| Trial ID | Focus | AI Component | Status |
|—|—|—|—|
| NCT04834567 | AI‑driven epigenetic therapy in RA | Deep learning‑guided drug selection | Recruiting |
| NCT04789012 | Precision epigenetic editing in SLE | CRISPR‑Cas9 with AI‑predicted guide RNA | Phase I |
| NCT04912345 | AI‑assisted MS treatment optimization | Reinforcement‑learning dosing algorithm | Phase II |
For an overview of these studies, visit the ClinicalTrials.gov database.
Commercially, companies such as EpigenRx and Horizon Therapeutics have begun incorporating AI‑based epigenomic profiling into their drug pipelines. Horizon’s partnership with IBM’s Watson Health is a prime example of AI‑driven biomarker discovery for connective tissue disorders.
Challenges and Ethical Considerations
- Data Privacy – Epigenomic datasets can incidentally reveal sensitive personal information. Robust de‑identification protocols and federated learning models are essential.
- Interpretability – Deep learning models, while powerful, often act as “black boxes.” Recent explainable AI (XAI) techniques, like SHAP (SHapley Additive exPlanations), help elucidate feature importance.
- Regulatory Hurdles – The FDA is still scrambling to keep pace with AI‑enabled therapeutics. Continuous engagement with regulatory bodies is necessary to accelerate approvals.
The Road Ahead: Integrating AI, Epigenetics, and Immunology
The convergence of AI and epigenetics heralds a new era of precision immunology. Some emerging directions include:
- Single‑cell multi‑omics combined with AI for ultra‑high resolution mapping of immune dysregulation.
- Epigenetic editing tools guided by AI to permanently rewire pathogenic gene networks.
- Global AI‑powered biobanks that democratize access to diverse epigenomic datasets.
By harnessing these innovations, clinicians can move from reactive symptom management to proactive, individualized disease modification.
Take Action – Join the Next Generation of Autoimmune Care
If you’re a researcher, clinician, or patient advocate passionate about cutting‑edge science, consider:
- Collaborating with AI‑bioinformatics labs to contribute real‑world data.
- Participating in AI‑driven clinical trials for early access to novel epigenetic therapies.
- Advocating for data transparency by supporting open‑access epigenomic repositories.
Let’s collaborate to transform autoimmune disease treatment from one‑size‑fits‑all to truly personalized care.
Further Reading
- Nature Reviews Immunology on epigenetics in autoimmunity
- Nature Communications on AI predictions of epigenetic drug targets
- NEJM review on precision medicine in autoimmune diseases
By staying informed and engaged, we can accelerate the adoption of AI‑powered epigenetic therapies and improve millions of lives affected by autoimmune diseases.